SCIENTIFIC REPORT
“Reference values of intraocular pressure measured by EASYTON tonometer and Goldman tonometer for eyelids with epicanthic fold (Mongolian fold) in residents of Kazakhstan”
Objective: To perform a comparative assessment of the IOP measurement using EASYTON tonometer and Goldman tonometer for the eyes with an epicanthic eyelid fold – Mongolian race representatives (residents of Kazakhstan).
A characteristic feature of Mongoloid/Mongolian races, also found in Northern Europe and in countries like Ireland, is the so-called epicanthic or Mongolian fold, a fold in the upper eyelid in the innermost corner of the eye. To a greater or lesser extent, it covers the lacrimal tubercle. This is particularly concentrated in representatives of the Central Asian mongoloid races, though it is also found to a lesser extent in many other ethnic groups around the world. This study set out to ascertain if the epicanthic fold impacts on IOP measurement through the eyelid.
Material and methods.
The IOP measurements were carried out in the Eye Microsurgery Public State Enterprise (with the Right of Economic Management) “The Prof. H.Zh.Makazhanov Polyclinic No. 1” of Karaganda city and the «TENSV Clinic» LLP – the clinical bases of the Ophthalmologic Chair of the Medical University of Karaganda (MUK).
150 patients (150 eyes) were examined overall. For each patient, IOP was initially measured with the Goldman tonometer and then with the EASYTON tonometer. The study was conducted under the provisions of ISO 8612.
In total, the 150 reference IOP measurements were categorized in the following 4 ranges:
- Under 17 mmHg: 40 measurements;
- 17 – 23 mmHg: 40 measurements;
- Above 23 mmHg: 40 measurements;
- High astigmatism: 30 measurements.
The IOP measurement procedure consisted of the following steps:
- Removal of the tonometer from its case
- The device was held so that the sensor rod faced upwards and the protective cap was removed.
- The tonometer was switched on by briefly depressing the power button. The tonometer’s readiness for operation was indicated by an arrow on the display.
- The functionality of the tonometer was then confirmed using the provided control device.
- The tonometer rod and protective ring were disinfected via an antiseptic swab.
- The tonometer was then turned so that the measuring rod faced downwards and the display was visible.
- We operators positioned ourselves to the side and back of the patient.
- The patient’s sight was set and focused on a test object (usually the patient’s own hand) so that his/her line of sight approximated a 45-50° angle.
- The palmar base of the hand holding the tonometer rested on the patient’s forehead. The consistency and accuracy of movements during measurement was achieved by supporting the patient’s forehead with the hand holding the tonometer, as well as by practicing the measurement technique.
- The upper eyelid was unfolded with a finger of the free hand, such that the edge of the upper eyelid coincided with the eyelid limb. We kept the eyelid in this position and didn’t permit it to shift towards the cornea when measuring! However, we didn’t apply pressure to the eyeball.
- The contact area of the tonometer rod was in the upper portion of the sclera corresponding to the corona ciliaris in the 12 hours meridian.
The device rod was gently set on the eyelid 2-3 millimeters above the edge of the lid and above the upper border of the iris. Holding the tonometer upright, the rod was gently depressed by 2-3 mm. The dynamic impact was experienced like soft vibration. During the measurements it was ensured that the protective ring of the tonometer did not touch the eyelid, and remained 2-3 mm from the eyelid.
If the tonometer is depressed too much, the tonometer emits a continuous monophonic sound signal that ceases when the tonometer is raised to a level that is appropriate for measurement.
- 1-2 seconds after the start of the measurement, the tonometer generated an audio signal indicating that measurement was done. To complete the measurement, the instrument was gently lifted. After completion, another sound signal was emitted and the measured value of the IOP was shown on the tonometer’s display.
- If no sound signal occurs, or if it is delayed by more than 3 seconds, the measurement should be repeated.
- The tonometer was switched off by briefly pressing the power button.
- After switching off, the outer surfaces of the device’s case, protective cap, protective ring and the portion of the vibrator rod protruding beyond the ring were disinfected.
The measurement results were grouped according to the 4 above ranges and are included in tabellar and graphic form in the report below.
Study authors
Head of the Opthalmology Chair of the Medical University of Karaganda (MUK).
Holder of Habilitation Degree in Medicine, Professor, Doctor of higher category
Shousterov Y.A.
Head of Unit,
Ocular Microsurgery and Chief ophthalmologist of Karaganda Region,
D.E. Toksambaeva
Table 1. IOP results obtained using EASYTON tonometer compared to Goldmann tonometer
| Table 1. Patients with IOP below 17 mmHg | |||||
| Patient No. | Goldman tonometer | EASYTON | Patient No. | Goldman tonometer | EASYTON |
| 1 | 10 | 10 | 21 | 16 | 16 |
| 2 | 11 | 10 | 22 | 16 | 16 |
| 3 | 11 | 12 | 23 | 16 | 18 |
| 4 | 11 | 10 | 24 | 16 | 15 |
| 5 | 11 | 12 | 25 | 16 | 17 |
| 6 | 12 | 12 | 26 | 16 | 16 |
| 7 | 12 | 13 | 27 | 16 | 18 |
| 8 | 12 | 12 | 28 | 16 | 16 |
| 9 | 13 | 13 | 29 | 16 | 16 |
| 10 | 13 | 12 | 30 | 16 | 18 |
| 11 | 13 | 13 | 31 | 16 | 16 |
| 12 | 13 | 12 | 32 | 16 | 17 |
| 13 | 14 | 14 | 33 | 16 | 16 |
| 14 | 14 | 15 | 34 | 16 | 16 |
| 15 | 14 | 15 | 35 | 16 | 16 |
| 16 | 15 | 14 | 36 | 16 | 16 |
| 17 | 15 | 16 | 37 | 16 | 16 |
| 18 | 15 | 15 | 38 | 16 | 16 |
| 19 | 15 | 16 | 39 | 16 | 17 |
| 20 | 15 | 15 | 40 | 16 | 15 |
Table 2: IOP results obtained using EASYTON tonometer compared to Goldmann tonometer
| Table 2. Patients with IOP in the range 17 to 23 mmHg | |||||
| Patient No. | Goldman tonometer | EASYTON | Patient No. | Goldman tonometer | EASYTON |
| 1 | 17 | 16 | 21 | 19 | 20 |
| 2 | 17 | 20 | 22 | 20 | 20 |
| 3 | 17 | 18 | 23 | 20 | 20 |
| 4 | 17 | 16 | 24 | 20 | 20 |
| 5 | 17 | 16 | 25 | 20 | 19 |
| 6 | 17 | 15 | 26 | 20 | 23 |
| 7 | 17 | 16 | 27 | 20 | 22 |
| 8 | 17 | 19 | 28 | 21 | 23 |
| 9 | 17 | 16 | 29 | 21 | 24 |
| 10 | 17 | 16 | 30 | 21 | 24 |
| 11 | 18 | 20 | 31 | 21 | 22 |
| 12 | 18 | 19 | 32 | 22 | 25 |
| 13 | 18 | 16 | 33 | 22 | 19 |
| 14 | 19 | 19 | 34 | 22 | 25 |
| 15 | 19 | 17 | 35 | 22 | 22 |
| 16 | 19 | 17 | 36 | 22 | 23 |
| 17 | 19 | 19 | 37 | 23 | 23 |
| 18 | 19 | 20 | 38 | 23 | 23 |
| 19 | 19 | 19 | 39 | 23 | 25 |
| 20 | 19 | 20 | 40 | 23 | 21 |
Table 3. IOP results obtained using EASYTON tonometer compared to Goldmann tonometer
| Table 3. Patients with IOP in the range above 23 mmHg | |||||
| Patient No. | Goldman
tonometer |
EASYTON | Patient No. | Goldman
tonometer |
EASYTON |
| 1 | 24 | 24 | 21 | 25 | 26 |
| 2 | 24 | 25 | 22 | 25 | 24 |
| 3 | 24 | 23 | 23 | 25 | 25 |
| 4 | 24 | 24 | 24 | 26 | 26 |
| 5 | 24 | 26 | 25 | 26 | 26 |
| 6 | 24 | 24 | 26 | 26 | 24 |
| 7 | 24 | 25 | 27 | 26 | 27 |
| 8 | 25 | 27 | 28 | 26 | 24 |
| 9 | 25 | 25 | 29 | 26 | 27 |
| 10 | 25 | 26 | 30 | 27 | 27 |
| 11 | 25 | 28 | 31 | 27 | 28 |
| 12 | 25 | 26 | 32 | 28 | 28 |
| 13 | 25 | 26 | 33 | 28 | 29 |
| 14 | 25 | 23 | 34 | 28 | 28 |
| 15 | 25 | 24 | 35 | 29 | 31 |
| 16 | 25 | 25 | 36 | 29 | 29 |
| 17 | 25 | 25 | 37 | 32 | 33 |
| 18 | 25 | 26 | 38 | 38 | 36 |
| 19 | 25 | 26 | 39 | 40 | 42 |
| 20 | 25 | 25 | 40 | 41 | 43 |
Correlation of IOP indicators obtained using the EASYTON tonometer and Goldman tonometer
Diagram 1
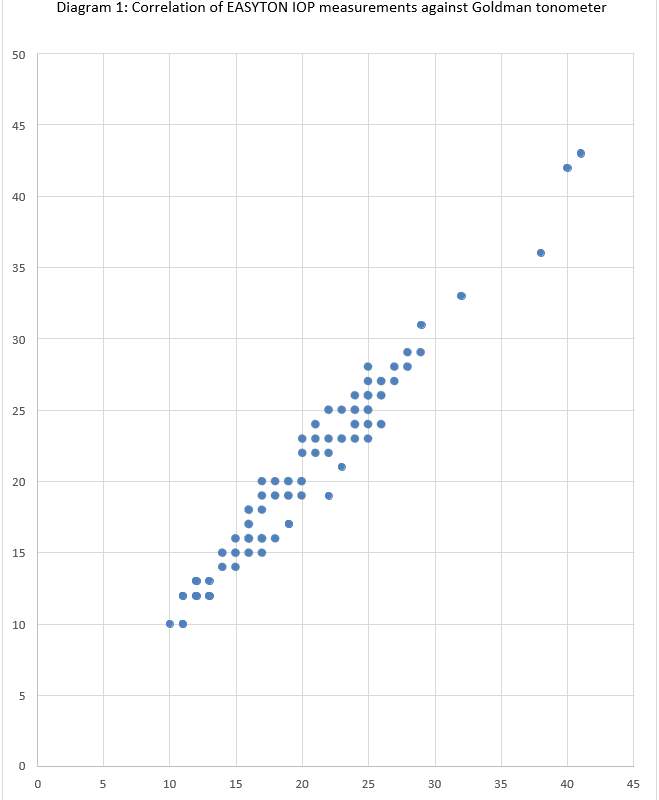
Table 4. The results of IOP measurements performed by EASYTON tonometer compared to those obtained using Goldman tonometer as a reference standard for patients with high astigmatism (over 3 diopters)
| Table 4a. Patients with high astigmatism and IOP under 17 mmHg | ||
| Test Object No. | Goldman tonometer | EASYTON |
| 1 | 14 | 14 |
| 2 | 15 | 14 |
| 3 | 15 | 16 |
| 4 | 15 | 17 |
| 5 | 16 | 17 |
| 6 | 16 | 18 |
| 7 | 16 | 16 |
| 8 | 16 | 18 |
| 9 | 16 | 17 |
| 10 | 16 | 16 |
| Table 4b. Patients with high astigmatism and IOP of 17 to 23 mmHg | ||
| Test object 11 | 17 | 19 |
| 12 | 17 | 17 |
| 13 | 17 | 18 |
| 14 | 17 | 19 |
| 15 | 18 | 20 |
| 16 | 18 | 20 |
| 17 | 20 | 22 |
| 18 | 21 | 20 |
| 19 | 22 | 24 |
| 20 | 23 | 22 |
| Table 4c. Patients with high astigmatism and IOP above 23 mmHg | ||
| Test object 21 | 24 | 25 |
| 22 | 24 | 26 |
| 23 | 25 | 23 |
| 24 | 25 | 26 |
| 25 | 25 | 27 |
| 26 | 26 | 26 |
| 27 | 27 | 29 |
| 28 | 31 | 30 |
| 29 | 31 | 32 |
| 30 | 32 | 32 |
Diagram 2. Correlation of IOP indicators obtained by EASYTON tonometer and Goldman tonometer in patients with high astigmatism
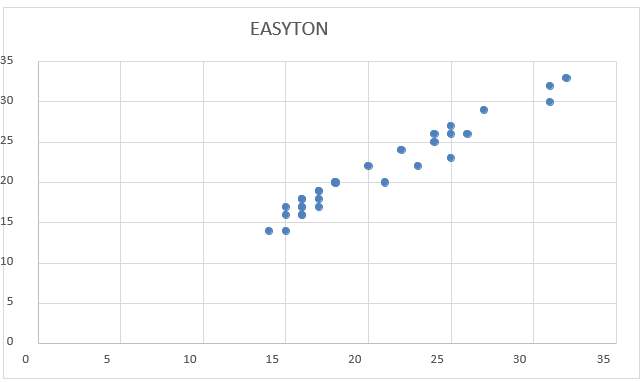
Conclusion: the measurements obtained using EASYTON tonometer are strongly correlated to the values obtained using the Goldman tonometer (see Diagrams 1, 2).
No particularities in the measurement of IOP were found in people with an eyelid epicanthic fold (Mongolian fold) in residents of Kazakhstan.
MINISTRY OF HEALTH CARE OF THE REPUBLIC OF KAZAKHSTAN
Public State Enterprise with the Right of Economic Management “The Prof. H.Zh.Makazhanov Polyclinic No. 1”
Approved
Director
D. T. Kurmangaliev
12/29/2019

 EN
EN